Clinical Nutrition Support for Patients with ARDS

The scope
- clinical dietitians as credentialed practitioners, involve in the management of patients, such as assessment of the nutritional status and plan the dietary needs of the patients. Follow up the nutrition status of the patients and the quality and safety of nutrition support in both hospitals and quarantines.
- The clinical dietitian, to fulfil his/her responsibilities cooperate and coordinate with the doctors in charge, dietitian general (food services), nurses and clinical pharmacists.
- Credentialed practitioners should ensure the duties being performed are within their individual scope of practice, and were trained to do so. Such as how to assess the nutritional status for critical ill patients in ICU and knew the skills of dealing with tube feeding accessories.
Dietary planning for ICU patients: – (ESPEN, Clinical Nutrition April 2020)
♣ Energy needs: – According to the ESPEN expert statement and practical guidance for nutritional management of SAR-COV 2 infection (April 2020) statement 2.
♣ Energy needs can be assessed using indirect calorimetry if safely available with ensured sterility of the measurement system, or as alternatives by prediction equations or weight-based formulae such as:
- 27 kcal per kg body weight and day; total energy expenditure for poly-morbid patients aged >65 years.
- 30 kcal per kg body weight and day; total energy expenditure for severely underweight poly-morbid patients.
- 30 kcal per kg body weight and day; guiding value for energy intake in older persons. This value should be individually adjusted with regard to nutritional status, physical activity level, disease status and tolerance
The target of 30 kcal/kg body weight in severely underweight patients should be cautiously and slowly achieved, as this is a population at high risk of refeeding syndrome. The society of Critical Care Medicine and the American Society of Parenteral and Enteral Nutrition, recommended that, feeding should be initiated with low dose and increase slowly to full dose to meet the energy requirement within one week (Robert et al, 2020).
♣ Protein needs: – Usually estimated using formulae such as:
- 1 g protein /kg body weight/day in older persons. The amount should be individually adjusted with regard to nutritional status, physical activity level, disease status and tolerance.
- >1 g protein / kg body weight / day in poly-morbid medical inpatients, may reach 20% of total calorie, in order to prevent body weight loss, reduce the risk of complications and hospital readmission and improve functional outcome.
♣ Fat and carbohydrate need: – While considering an energy ratio from fat and carbohydrates between 30:70 (subjects with no respiratory deficiency) to 50% to 50% for ventilated patients.
♣ Vitamins, mineral and antioxidants
Vitamins and mineral should be individually adjusted. According to the ESPEN expert statement and practical guidance for nutritional management of SARCOV 2 infection (Robert et al ., 2020) statement 3, stated that, subjects with malnutrition should ensure sufficient supplementation with vitamin and minerals.
♣ Formula with a higher caloric density
Patients with pulmonary disease resulting in CO2 retention, such as chronic obstructive pulmonary disease or respiratory failure, may benefit from water restriction. Therefore, a formula with a higher caloric density may be helpful in these situations.
3:2- Recommendation 2: Timing of Nutrition Delivery (ASPEN April 2020)
The aim should be to initiate early enteral nutrition (EN) within 24-36 hours of admission to the ICU or within 12 hours of intubation and placement mechanical ventilation, the patient with sepsis or circulatory shock can tolerate trophic feeding (a small volume of balanced enteral nutrition insufficient for the patient’s nutritional needs but producing some positive gastrointestinal or systemic benefit). The shifting to parenteral nutrition should be lowered.
(ESPEN, Clinical Nutrition April 2020) statement
-
- Nutritional treatment should start early during hospitalization (within 24-48 hours). Especially for older and poly-morbid patients whose nutritional conditions may be already compromised, nutritional treatment and targets should be met gradually to prevent refeeding syndrome Oral nutritional supplements (ONS) should be used whenever possible to meet patient’s needs, when dietary counselling and food fortification are not sufficient to increase dietary intake and reach nutritional goals, ONS shall provide at least 400 kcal/day including 30 g or more of protein/day and shall be continued for at least one month. Efficacy and expected benefit of ONS shall be assessed once a month.
3:3- Recommendation3: Route, Tube Placement & Method of Feedings
Generally, there are three methods of feedings
- Oral feeding.
- Enteral or tube feeding for those who cannot eat normally and the gastrointestinal tract all or part of is functioning normally. This type of feeding profession expert in tube feeding.
- Parenteral feeding: – Need profession expert
3:3:1 -Indications of tube feeding
- Patients who cannot or will not eat.
- Patients who have a functional gut.
- Safe method of access is possible.
Methods to administer tube feedings:
- Continuous Drip Feeding: – The continuous drip method is most commonly used, is administered via gravity or a pump and is usually tolerated better than bolus feedings.
- Bolus Feedings: – Bolus feedings allow for more mobility than continuous drip feedings.
- Combination: – A combination of continuous drip (at night) and bolus feedings (during the day) can be used.
Patients with COVID-19, enteral nutrition is preferred to parenteral nutrition. Infusion of formula into the stomach feeding nasogastric tube requires minimal expertise. If gastric feeding is unsuccessful due to enteral feeding intolerance, use of a prokinetic agent to enhance motility is recommended as the second step. Post pyloric EN delivery is recommended only after these strategies fail. Placement of any enteral access device may provoke coughing and should be considered an aerosol generating procedure. If possible, keep the patient’s mouth covered during
placement in the nares and follow CDC guidelines regarding the use of N-95 masks and PAPR during tube placement. Lastly, placement of post-pyloric feeding tubes may take longer to place than gastric tubes, increasing exposure time of the healthcare practitioner.
Early EN may not be preferential in a subset of patients with COVID-19 with gastrointestinal (GI)involvement, before the onset of respiratory symptoms, some patients initially present with diarrhea, nausea, vomiting, abdominal discomfort and in some cases gastrointestinal bleeding. when present early use of PN should be considered, transitioning to EN when GI symptoms subside.
In poly-morbid medical inpatients and in older persons with reasonable prognosis, the nutritional requirements cannot be met orally, enteral nutrition (EN) should be administered. Parenteral nutrition (PN) should be considered when EN is not indicated or unable to reach targets.
Delivery System (Open or Close Tube Feeding)

Depending on how a tube-feeding product is packaged, infusion is via an open or closed delivery system.
- The open system utilizes either a large syringe or an open-top container for tube-feeding delivery. Products include flip-top cans, bottles, brick packs, or powder packages that require reconstitution with water (at formula room).
- The closed system, a container is prefilled with the sterilized tube-feeding product; the bottle then is spiked with tubing and attached to the enteral access device.
The container usually contains at least 1 L of product and formula hang time is usually between 24 and 36 hours, as long as sterile technique is used.
Patients with COVID-19, in ICU unit, closed system tube feeding is recommended, if the suitable nutrition formulas are available.
ESPEN, Clinical Nutrition April 2020 statement
In poly-morbid medical inpatients and in older persons with reasonable prognosis, whose nutritional requirements cannot be met orally, enteral nutrition (EN) should be administered.
Parenteral nutrition (PN) should be considered when EN is not indicated or unable to reach targets.
Enteral nutrition should be implemented when nutritional needs cannot be met by the oral route, e.g. if oral intake is expected to be impossible for more than three days or expected to be below half of energy requirements for more than one week. In these cases, the use of EN may be superior to PN, because of a lower risk of infectious and non-infectious complications
Monitoring for EN potential complications should be performed.
In COVID-19 non-intubated ICU patients not reaching the energy target with an oral diet, oral nutritional supplements (ONS) should be considered first and then enteral nutrition treatment. If there are limitations for the enteral route, it could be advised to prescribe peripheral parenteral nutrition in the population not reaching energy-protein target by oral or enteral nutrition.
In COVID-19 intubated and ventilated ICU patient’s enteral nutrition (EN) should be started through a nasogastric tube; post-pyloric feeding should be performed in patients with gastric intolerance after prokinetic treatment or in patients at high-risk for aspiration; the prone position per se does not represent a limitation or contraindication for EN.
Continuous rather than bolus EN should be used.
Five studies were identified and ESPEN Meta-analysis found a significant reduction in diarrhea with continuous versus bolus administration
In patients with gastric feeding intolerance not solved with prokinetic agents, post pyloric feeding should be used.
In critically ill patients with gastric feeding intolerance, intravenous erythromycin should be used as a first line prokinetic therapy.
Alternatively, intravenous metoclopramide or a combination of metoclopramide and erythromycin can be used as a prokinetic therapy.
Gastric access should be used as the standard approach to initiate EN.
In patients deemed to be at high risk for aspiration, post pyloric, mainly jejunal feeding can be performed.
3:4- Recommendation 4: Nutrition Dose, Advancing to Goal and Adjustments
With mild symptoms normal dietary intake. When patients admitted to ICU unit. Feeding should be initiated with low dose EN (hypochromic or trophic diet). Increase slowly to full dose to meet the energy requirement within one week. To reach 15- 20 kcal/kg/day actual body weight, which should be 70 to 80% of the total calorie. Protein goal of 1.2- 2.0 gram/kg/day (actual body weight) for ICU patients.
In ICU patients with dysphagia, texture-adapted food can be considered after extubation if swallowing is proven unsafe, EN should be administered. In cases with a very high aspiration risk, post pyloric EN or, if not possible, temporary PN during swallowing training with removed nasoenteral tube can be performed.
EN should be withheld in the patient with hemodynamic instability requiring vasopressor support at high or escalating doses, patients on multiple vasopressor agents, or rising lactate levels. EN may be initiated or restarted after the patient is adequately resuscitated and/or has been on a stable vasopressor dose with sustained mean arterial blood pressure of ≥ 65 mmHg (Robert et al., 2020).
EN should be held and PN strongly considered in patients with gastrointestinal intolerance such as abdominal pain, nausea, diarrhea, significant abdominal distension, dilated loops of small and large bowel with air/fluid levels, pneumatosis intestinalis or increasing nasogastric outputs in previous 6- 12 hours with start of trophic feeds or prior to initiation of EN (Robert et al., 2020).
Enteral Nutrition in the Mechanically Ventilated Patient.
Mechanically ventilated patients are unable to take food orally and therefore are dependent on enteral nutrition for provision of energy and protein and other nutrients requirements. Enteral nutrition is supportive therapy and may impact patient outcomes in the intensive care unit. Early enteral nutrition has been shown to decrease complications and hospital length of stay and improve the prognosis at discharge (Allen and Hoffman., 2019, Todd et al., 2011).
Recommendation 5: Formula Selection

3:5:1- The important of choosing the appropriate formula
- Proper nutrition is needed for anabolism, recovery and maintenance of optimal nutritional status.
- Formula selection is critical to the success of nutrition therapy, both in terms of satisfying metabolic requirements and increasing gastrointestinal tolerance.
- Before initiating feeding, select an appropriate formula based on the patient’s specific needs
- It is important to know the formula contents.
3:5:2- Steps to select the appropriate formula
- Evaluate the nutritional status
- Determine the amount of nutrients needed
- Discuss with the doctor in charge to determine the route of feeding.
- Select the appropriate nutrition formula(s).
Categories of Enteral Formulas
- Polymeric formulas either Commercial or Blenderized
- Oligomeric formulas.
- Disease-specific formulas.
- Modular formulas (concentrated protein and carbohydrate preparations) to enhance protein and caloric content of enteral formulas.
- Standard: Intact protein, “meal replacement”, may contain fiber or hydrolyzed/Pre-Digested- Protein typically small peptides.
3:5:3- Formula suitable for pulmonary disease with CO2 retention (Mechanical Ventilation)
Formula clinically significant in reducing CO2 production called Pulmonary Formulas
- Formula low in carbohydrate and high in fat content while reducing CO2 production.
- Decreased carbohydrate content and increased fat content (Provide high energy and produce less CO2)
- High caloric density with intact proteins and fiber supplement.
- Some formula contains Eicosapentaenoic acid, gamma-linolenic acid, antioxidants no arginine supplementation.
3:5:4- Formula Room: –
To reduce the risk of infection. It is preferred to have the formula room, away from patients’ side. It could be located in the nutrition department (Kitchen) of the hospital The needs for formula room: –
- Powder nutrition formula need reconstitution with water.
- Use of more than one formula especially for open tube feeding system.
- Addition of food supplement, antioxidants or medicine
3:6- Recommendation 6: Monitoring Nutrition Tolerance
Evaluation of delivery of enteral nutrition in mechanically ventilated ICU patients is very important(Keng et al., 2014). Gastric residual volume (GRV) monitoring is not reliable for monitoring nutrition tolerance (Elke et al., 2015). Recoding the protein and calories intake on daily basis.
Gastric residual volume should not be used to avoid the risk of aspiration pneumonia. Patients should be monitored by laboratory investigations and passage of stool and gas.
3:6:1 Complications of tube feeding to be monitor
- Infection
- Aspiration
- Diarrhea
- Metabolic disturbances.
- Refeeding syndrome
- Alterations in drug absorption and metabolism.
The complications should be minimized. In case of refeeding syndrome, 25% of caloric goal should be started, in either enteral feeding if not possible then parenteral nutrition. The assessment of serum phosphate, magnesium and potassium levels to monitor their levels. The calories are slowly increased.
Treating respiratory distress is a priority when managing critically ill patients. Non-invasive ventilation (NIV) is increasingly used as a tool to prevent endotracheal intubation. Providing oral or enteral nutritional support during NIV may be perceived as unsafe because of the possible risk of aspiration so that these patients are frequently denied adequate caloric and protein intake.
Newly available therapies, such as high-flow nasal oxygen (HFNO) may allow for more appropriate oral feeding (Pierre and Rattanachaiwong., 2018).
To eat or to breathe? The answer is both! Nutritional management during noninvasive ventilation.
(ESPEN, Clinical Nutrition April 2020) statement
When patients are stabilized and even in prone position, enteral feeding can be started ideally after measuring indirect
Calorimetry targeting energy supply to 30% of the measured energy expenditure.
Energy administration will be increased progressively. During emergency times, the predictive equation recommending 20 kcal/kg/day could be used and energy increased to 50-70% of the predictive energy at day 2 to reach 80-100% at day4
The protein target of 1.3 g/kg/day should also be reached by day 3-5. Gastric 374 tube is preferred but in case of large gastric residual volume (above 500 mL), duodenal tube should be inserted quickly.
The use of enteral omega-3 fatty acids may improve oxygenation but strong evidence is missing. If intolerance to enteral nutrition is present, parenteral nutrition should be considered.
Blood glucose should be maintained at target levels between 6-8 mmol/l, along with monitoring of blood triglycerides and electrolytes including phosphate, potassium and magnesium.
3:8- Recommendation 8: Nutrition Therapy During ECMO (ASPEN April 2020) recommendation
One of the major barriers to Extracorporeal membrane oxygenation (ECMO). Enteral nutrition for patients with ECMO may be safe and tolerated. Study of patients with ECMO having EN found that 4.5% developed bowel ischemia.
Post-mechanical ventilation period and dysphagia
(ESPEN, Clinical Nutrition April 2020) statement
Patients no longer needing mechanical ventilation have high incidence of swallowingproblems and consequent dysphagia which may strongly limit oral nutrient intake, even at a time of general improvement of clinical conditions..
In ICU patients with dysphagia, texture-adapted food can be considered after extubation. If swallowing is proven unsafe, EN should be administered. In cases with Avery high aspiration risk, post pyloric EN or, if not possible, temporary PN during swallowing training with removed nasoenteral tube can be performed.
The post-extubation swallowing disorder could be prolonged for to up to 21 daysmainly in the elderly and after prolonged intubation , which makes this complication particularly relevant for COVID-19 patients
The presence of severe post extubation dysphagia was associated with severe outcome including pneumonia, reintubation and hospital mortality. Recently ICU patients had prolonged post extubation swallowing disorder at discharge and some post extubation swallowing disorder has been shown 4 months after dischargeIt is recommended referring patients recognized to have swallowing issues for swallowing evaluation, in order to prevent oral nutrition complications.

50 Years Old Male Patient Referred To Us From Al Abeer Polyclinics On 17-4-2023 WITH P/H OF HTN-DM ((stopped medications)) Presented with low grade fever, hypotension, severe leukopenia and elevated liver functions for further investigations and management PT started IV fluids and necessary investigations Which Showed>>>>Showed TYPE2 DM. high HBA1C.high bilirubinaemia, elevated liver function tests, high creatinine and severe leukopenia WBCS=0.6 ECHO showed EF=40, CXR showed cardiomegaly and consolidation with bilateral pleural effusion, dyspnoea and hypoxemia Admitted at ICU on mechanical ventilation. pan cultures withdrawn, started immediately Empirical antibiotics, insulin infusion and high dose inotrope started. CT CHEST done showed Bilateral Consolidation, ARDS (Acute respiratory distress syndrome) and effusion Labs Showed Hypernatremia, Thrombocytopenia and Acute Kidney Injury Patient Given Dose Adjustment IV meds as per KFTS Given Also IV Albumin and Platelets Transfusion Culture Based IV Tazocin, Levofloxacin and Flagyl Anticoagulant Given With Dose Adjustment. On DVT Machine, Air Mattress Creatinine returned to normal Then weaning from inotropes Cardiology, Chest. Nephrology, Neurological, Surgery and Haematology Consultations Done Adding Medications CT chest follow up 2-5-2023 Showed ARDS, Massive Bilateral Consolidation, Bullae, Bilateral Effusion and RT Side Pneumothorax Cardiothoracic Consultation Done >>>Visited the Patient and Inserted RT Chest Tube >>> IV Triple Antibiotics Received Including Double Antipseudomonal and Anti Versa, patient then improved clinically and radiology , trial weaning from mechanical ventilation done several times but failed , then tracheostomy done and then weaned from mechanical ventilation , but has frequent attacks of tachypnea , desaturation due to accumulation of secretions and blood clots , he has also generalizes muscle weakness cannot move any part of body , undergo chest physiotherapy and frequent suction of secretion , chest tube is removed , still nasogastric tube feeding and tracheostomy with oxygen.
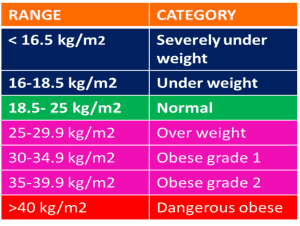
A anthropometry 1- weight = 67 kg 2-Height = 168 cm (1.68 m) 3- BMI = 67/2.82 = 23.75 kg /m2
Disease-Specific Formula (Pulmonary)
So this patient is non obese and we’ll calculate the actual BW
weight loss = 13/67 X 100 = 19.40% from his weight
> 15 % from his weight so severely malnourished
→mild from if loss 5-7% from body weight.
→Moderate if loss from 7- 15 % from body weight.
→Sever if loss > 15% from body weight classified as sever.
- Mr Artemio was assessed as being severely malnourished
- At high risk of re-feeding syndrome.
- recommend Nasogastric feeding by the medical team
- as Mr Artemio is not safe for oral intake and his intake is not adequate to meet nutritional requirements.
Question : determine the nutritional requirements for this patient
calculate energy and protein, fluid requirements ♠
- BEE is easily estimated by the equation BEE =25 x wt body weight (kg)
- Hypercaloric feeding significantly increases the production of CO2
- 25 x 67 = 1675 kcal/d
- Total daily expenditure =BEE x activity factor x injury factor
- = 1675 x 1 x 1.2 = 2010 kcal /day = fluid requirements
- Protein = 67 x 1.6 = 107 gm / day
♠ Fat and carbohydrate
- IV fat emulsions may decrease arterial oxygenation
- Pre-existing lung injury such as ARDS may potentiate the adverse effect of intravenous fat emulsion
- high-fat, low-carbohydrate diet can significantly reduce VO2and ultimately reduce PCO2
- This is particularly useful in patients on mechanical ventilation who are difficult to wean with high PCO2and VCO2 levels, because of the difficulty eliminating carbon dioxide
- high fat, low carbohydrate – enteral formulas were developed for pulmonary failure patients
- Current practice emphasizes provision of measured or estimated energy requirements rather than hyperalimentation or high fat formulations.
- Propofol (10% fat emulsion) is a frequently used sedative for mechanically ventilated patients, so it must be calculated in the total fat requirements.
- There is limited evidence that pulmonary formulas have clinically significant benefits compared to standard or nutrient-dense formulas that provide adequate energy, regardless of carbohydrate to fat ratio
♣ Nutrient Needs in Stable COPD
- Protein: 2-1.7 grams/kg (15-20% of calories) to restore lung and muscle strength and promote immune function
- Fat: 30-45% of calories
- Carbohydrate: 40-55% of calories
- Maintain appropriate RQ
♦ Vitamins and minerals
- Specific nutrients depleted in pulmonary disease include iron, vitamin A, vitamin C, vitamin E, and selenium
- Phosphorus is lower in patients with pulmonary conditions such as COPD
- Patients with advanced pulmonary disease are at risk for
low bone mineral density due to :
- glucocorticosteroid therapy
- reduced level of physical activity
- life-long smoking
- inadequate intake of vitamin D and calcium.
♣ Fluid
- Critically ill patients with pulmonary disease may need moderate to severe fluid restriction.
- Patients with respiratory problems often develop heart failure, which complicates the fluid replacement process
- For cor pulmonale, congestive heart failure, or ARDS, the nutrition regimen is generally delivered with concentrated calories and sodium-restricted formulas.
- Fluid overload often results in pulmonary congestion or edema, further complicating a poorly functioning lung
TABLE 26-3 A.S.P.E.N. Practice Guidelines for Pulmonary Failure”
- Patients with COPD or ARDS are at nutrition risk and should undergo nutrition screening to identify those who require formal nutrition assessment with development of a nutrition care plan.
- Energy intake should be kept at or below estimated needs in patients with pulmonary disease and demonstrated carbon dioxide retention.
- Routine use of modified carbohydrate and fat nutrition formulation in patients with pulmonary disease is not warranted.
- Provision of a modified enteral formulation containing n-3 fatty acids may be beneficial in the patient with early ARDS.
- A fluid-restricted nutrient formulation should be used in patients with ARDS whose hemodynamic status necessitates fluid restriction.
- Serum phosphate levels should be monitored closely in patients with pulmonary disease.
Nutrition in pulmonary diseases
Route of nutrition administration :Enteral route
- aspiration into the trachea is possible in case of nasogastric tube
- Cuffed endotracheal tubes may reduce the volume of aspirate, but do not prevent the complication.
- Small bowel feeding may prevent aspiration
- Antacid therapy is a major cause of diarrhea and should not be given to patients with acute respiratory failure
- Medications containing sorbitol, such as theophylline elixirs, also contribute to the incidence of diarrhea
Parenteral route
- If patients are fluid restricted, the parenteral nutrition solution will need to be concentrated.
- Once the patient has been weaned from mechanical ventilation, it is appropriate to gradually increase caloric intake above REE to promote a positive nitrogen balance and to replete nutrition deficits
Refeeding syndrome
- Hypophosphatemia can result in:
- decreased lung function
- Decrease in production of enzymes responsible for the release of oxygen from hemoglobin to the peripheral tissues and vital organs
- Diaphragmatic muscle weakness
- Acute respiratory failure
- Difficulty in ventilator weaning
Mechanical Ventilation and Weaning
- Increased carbon dioxide production from excessive carbohydrate intake and excessive total calories contributes to the inability to wean from mechanical ventilation
- Mechanical ventilation induces a gradual fluid retention after 48 to 72 hours on positive pressure ventilatory support
- Persistent positive fluid balance is associated with prolonged mechanical ventilation
- Weaning from mechanical ventilation depends on the patient’s ability to provide adequate gas exchange during spontaneous ventilation and the ability to achieve a patent upper airway
- Feeding regimens during the weaning period should focus on optimizing nutrient delivery without excessive calorie
Will you recommend continuous, intermittent, bolus feeding- why?
- Recommended regimen for enteral feeding:Continuous.Why?
As pt is not able to eat orally so therefore not able to meet requirements any other way.
High risk of aspiration and refeeding syndrome so need decreased slow feeding rate to reduce risk of aspiration, therefore continuous is most suitable. (If bolus feeding it would be at a much higher feeding rate which increases risk of aspiration)
What enteral route will you recommend and why?
- Enteral route? Directly into stomach via nasogastric tube.
- Why?
- Unknown diagnosis and therefore unsure how long NGF will be continued – therefore not recommended for PEG as this is for long term feeding
- No indication of malabsorption so therefore not indicated for post pyloric feeding ie: duodenal or jejunal feeding.
Before calculating the low rate for Mr,Artemio – what do you need to consider?
- IV Fluids
- Re-feeding risk
- Commence feeding at 50% pt requirements and increase gradually every 2nd day to reach goal in 1-2 weeks.
- (Enteral guidelines) Will need to recommend daily Thiamine administration 30 min prior to commencing feed and commence multivitamin.
- Daily blood test to ensure PO4, K, Mg are within normal limits and recommend replacement prior to feeding if low.
How will you monitor Mr Artemio. and assess for tolerance?
- Daily during the First week (re-feeding risk)
- – Electrolytes (spatially PO4, K, Mg) if low – recommend replacement
- – Tolerance to feed- e.g. nausea, vomiting, diarrhoea, constipation, abdominal discomfort, abdominal distension
- – Assess for signs of aspiration – reflux or vomiting feeds.
- – check bed position, tube position etc